Disorganized Attachment: When Safety and Threat Wear the Same Face

In the late 1980s, developmental psychologist Mary Main discovered something that shouldn't exist according to attachment theory. She found infants who, when reunited with their caregiver after a brief separation, would approach and then freeze mid-step. Or run toward their mother and then veer away. Or collapse to the ground crying without being able to move toward comfort. They looked, Main wrote, "like prey animals who have just seen a predator."
But the predator was the parent. The source of safety was simultaneously the source of threat.
Main called this disorganized attachment—the most chaotic and devastating attachment pattern. It represents what happens when an infant's fundamental drive to seek proximity to the caregiver directly conflicts with an equally fundamental drive to escape danger. The nervous system receives contradictory imperatives at the same time: approach and flee. Connect and withdraw.
From a polyvagal perspective, this is the catastrophic failure case. It's not anxious attachment (sympathetic hyperactivation) or avoidant attachment (sympathetic with learned suppression). It's the simultaneous activation of opposing autonomic states. Sympathetic arousal and dorsal vagal shutdown firing together.
This is what trauma looks like at the level of nervous system architecture. And understanding it reveals why some wounds don't heal through conventional means—why some people remain trapped in patterns that seem to defy logic.
The Polyvagal Money Shot
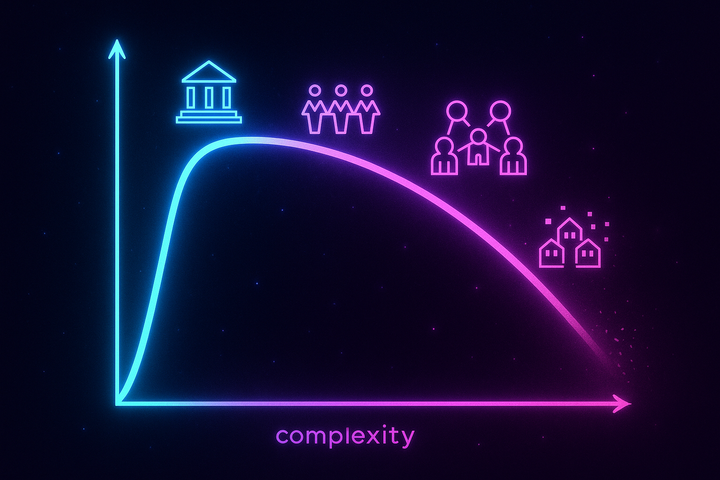
Polyvagal theory, developed by Stephen Porges, describes three hierarchical response systems in the autonomic nervous system:
1. Ventral vagal (social engagement) — "I'm safe, I can connect" 2. Sympathetic (mobilization) — "Fight or flight, I can escape" 3. Dorsal vagal (immobilization) — "Shutdown, freeze, play dead"
These systems typically operate in sequence. When you feel safe, ventral vagal dominates. When threat appears, you mobilize through sympathetic activation—your heart rate increases, blood flows to muscles, you prepare to fight or run. If escape is impossible, the older dorsal vagal system kicks in: metabolic shutdown, freeze, dissociation.
Disorganized attachment is what happens when sympathetic mobilization and dorsal immobilization fire at the same time.
It's the nervous system equivalent of pressing the gas and brake pedals simultaneously. The body wants to run and collapse at once. Approach and flee. Connect and shut down. The result is not a middle state—it's autonomic incoherence. A system at war with itself.
This is why disorganized attachment behaviors look so bizarre and fragmented. The infant approaches but can't complete the movement. Stretches arms toward the parent but turns their face away. Smiles while backing away. These aren't just confused behaviors—they're the body trying to execute mutually exclusive action patterns at the same time.
Main described it as "fright without solution." The child is terrified, but the source of fear is also the only source of comfort. There is no way out.
The Source of Chaos
Disorganized attachment doesn't develop from mere inconsistency or occasional stress. It develops when the caregiver is simultaneously the source of comfort and the source of terror.
This happens most commonly in three contexts:
1. Abuse or severe neglect — The parent who comforts is also the parent who hits, neglects, or terrifies. The infant learns that proximity brings both safety and danger.
2. Frightened or dissociative caregivers — Even without overt abuse, a parent who is themselves traumatized can create disorganized attachment. If the caregiver displays fear, dissociation, or emotional absence in the presence of the infant, the child picks up on this. They sense that the person who should provide safety is afraid—and fear is contagious. The infant becomes frightened of the caregiver's fear.
3. Unresolved trauma in the caregiver — Mary Main's Adult Attachment Interview revealed that parents with unresolved trauma—particularly around loss or their own abuse—are highly likely to have disorganized children. These parents may be loving and well-intentioned, but unprocessed trauma leaks out in subtle lapses of presence, sudden emotional shifts, or moments of dissociation that the infant's nervous system reads as danger.
The common thread: the attachment figure becomes paradoxical. They are safe and dangerous, present and absent, soothing and frightening. The infant's nervous system cannot form a coherent model. Prediction becomes impossible.
In AToM terms, M = C/T collapses. When Tension (T) is maximal—when the same stimulus predicts opposite outcomes—Coherence (C) cannot be maintained. The system fractures.
What Disorganized Attachment Looks Like
In Childhood
Mary Main's Strange Situation observations showed infants displaying:
- Contradictory behaviors — Approaching with head averted, backing toward parent, or approaching and then veering away at the last moment - Misdirected or interrupted movements — Reaching for the parent and then suddenly stopping mid-gesture, as if the body forgot what it was doing - Freezing or dissociation — Complete stillness for prolonged periods, blank stares, appearing to "go away" mentally - Stereotyped movements — Rocking, hair pulling, or other self-soothing behaviors that look mechanical and compulsive - Disorientation — Wandering aimlessly, confusion, lack of organized strategy for seeking comfort
The hallmark is the absence of a coherent strategy. Anxious children cling and protest. Avoidant children turn away and self-soothe. Disorganized children do both and neither. They oscillate, freeze, collapse, or simply fall apart.
In Adulthood
Disorganized attachment doesn't disappear with age. It shifts.
Adults with disorganized attachment histories often experience:
- Fearful-avoidant patterns — Simultaneous craving for closeness and terror of it. Relationships feel necessary and unbearable at once. - Extreme emotional dysregulation — Swings between rage, despair, numbness, and panic. Emotional states shift rapidly and unpredictably. - Dissociation under stress — "Spacing out," feeling numb, losing time, or experiencing oneself from a distance when relational threat appears. - Relational chaos — Push-pull dynamics, where they desperately seek connection and then sabotage it the moment it appears. Relationships become sites of compulsive reenactment. - Difficulty with emotional coherence — Trouble holding a stable sense of self or others. People flip between "all good" and "all bad" with little middle ground (splitting). - Chronic hypervigilance mixed with numbness — Wired and dead at the same time. Always scanning for danger but feeling nothing, or feeling too much and shutting down.
This is the long tail of autonomic incoherence. The nervous system never learned to settle into a single, coherent state. Instead, it remains trapped in the contradictory firing patterns that were adaptive—barely—in an environment where the caregiver was both haven and hazard.
The Neurobiology of Simultaneous Firing
What happens in the brain and body when sympathetic and dorsal vagal systems activate together?
Sympathetic activation increases heart rate, mobilizes energy, sends blood to large muscles, sharpens attention toward threat. It's a state of readiness—I can do something about this.
Dorsal vagal activation decreases heart rate, slows metabolism, reduces muscle tone, narrows attention to internal cues or blanks it out entirely. It's a state of surrender—nothing I do will help, so I'll shut down and wait.
When both systems fire at once:
- Heart rate becomes erratic — Rapid beats interspersed with sudden drops. Heart rate variability (HRV) becomes chaotic rather than rhythmic. - Muscle tone collapses while adrenaline surges — The person feels both wired and immobilized. Internally agitated but externally frozen. - Cognitive processing fragments — Attention scatters. Memory encoding becomes unstable. The person struggles to form a coherent narrative of what's happening. - Emotional experience becomes contradictory — Fear mixed with numbness. Rage without the ability to act. Grief that can't be felt or expressed.
This is not a stable state. It's a failure of integration. The polyvagal hierarchy—designed to shift smoothly between states depending on context—instead becomes a battlefield where incompatible systems fight for control.
In neuroimaging studies, individuals with disorganized attachment histories show reduced connectivity between prefrontal regulatory regions and limbic threat-detection regions. The top-down regulation that would normally resolve autonomic conflict doesn't function well. The systems remain stuck in simultaneous activation, with no executive override to choose one strategy and commit to it.
Fright Without Solution: The Impossible Bind
Disorganized attachment is what developmental trauma researchers call a "biological paradox." The infant's survival depends on proximity to the caregiver. But proximity triggers fear. Seeking safety activates the threat response.
This is not a psychological problem. It's a systemic coherence failure.
John Bowlby, the founder of attachment theory, argued that the attachment system has a single, overriding goal: maintain proximity to the caregiver in times of need. If that fails, the infant protests (anxious attachment). If proximity is consistently unavailable, the infant learns to suppress the drive (avoidant attachment).
But in disorganized attachment, the system cannot resolve the contradiction. The goal is both achieved and thwarted by the same action. Approaching the caregiver brings relief and danger. Distance brings safety and abandonment.
The nervous system has no algorithm for this. No coherent strategy. What emerges instead is chaos: fragmented behaviors, dissociation, a flickering between contradictory states.
Allan Schore, a leading researcher in interpersonal neurobiology, describes this as "relational trauma." The infant's developing brain is organized through co-regulation with the caregiver. When that caregiver is a source of dysregulation, the infant's brain cannot form stable regulatory patterns. Instead, it internalizes the chaos.
Porges describes disorganized attachment in polyvagal terms as a failure of neuroception—the unconscious detection of safety or danger. In typical development, neuroception becomes increasingly accurate. The child learns to distinguish real threat from false alarms. But when the caregiver's signals are contradictory—warm one moment, terrifying the next—neuroception becomes unreliable. The nervous system learns that everything is potentially dangerous, including the people meant to provide safety.
The result is a nervous system in perpetual crisis. Sympathetic arousal (mobilize!) and dorsal shutdown (immobilize!) fire simultaneously because the environment trained the system to expect both. The contradiction is internalized. The solution is, literally, impossible.
Dissociation as the Escape Hatch
If you can't approach and you can't flee, what's left?
You leave your body.
Dissociation—the felt sense of being disconnected from oneself, one's body, or reality—is the ultimate escape when external escape is impossible. It's the dorsal vagal system's last-ditch strategy: if I can't get away physically, I'll get away psychologically.
In disorganized attachment, dissociation becomes chronic. The infant learns that when proximity to the caregiver triggers simultaneous arousal and shutdown, the only way to survive is to "go away" mentally. To not be fully present in the body that's experiencing the contradiction.
This shows up in adulthood as:
- Depersonalization — Feeling like you're watching yourself from outside, like an actor in your own life - Derealization — The world feels fake, distant, dreamlike, or unreal - Emotional numbing — Inability to access feelings, even when intellectually aware that something significant is happening - Memory gaps — Losing time, not remembering conversations or events, experiencing oneself as discontinuous - Fragmentation of identity — Feeling like different "parts" of the self that don't communicate, as seen in dissociative identity disorder (DID), which is strongly linked to early disorganized attachment
From a polyvagal lens, dissociation is dorsal vagal dominance as a defensive strategy. When simultaneous firing becomes unbearable, the system tips fully into shutdown. Consciousness narrows, the body becomes distant, and the person retreats into an internal void where nothing—good or bad—can reach them.
It's a tragic adaptation. The child learns to survive by not being fully present. The cost is that they carry this strategy into adulthood, where relationships—even safe ones—trigger the same autonomic cascade. Closeness becomes intolerable not because the person is dangerous, but because the nervous system has learned that closeness always was.
The Geometry of Incoherence
In AToM's coherence geometry framework, disorganized attachment represents maximal curvature—the state space has become so unstable that small shifts trigger extreme, unpredictable changes.
When the caregiver's behavior is unpredictable and contradictory, the infant cannot form a stable attractor. There's no "home base" in state space, no configuration the nervous system can return to that feels safe and coherent.
Instead, the system cycles between multiple incompatible attractors:
- Sympathetic arousal (fight/flight) - Dorsal shutdown (freeze/dissociate) - Ventral engagement (connect/co-regulate)
But these attractors are not smoothly connected. The system doesn't transition between them in a predictable way. Instead, it jumps chaotically—from hyperarousal to shutdown to engagement and back, with no clear pattern.
In dynamical systems terms, this is a chaotic attractor. The trajectory through state space is hypersensitive to initial conditions. Tiny changes in context trigger wildly different responses. The person cannot predict their own reactions. They are dysregulated not just emotionally, but structurally.
Coherence—M = C/T—is minimal. The Tension (T) is overwhelming (caregiver as both threat and safety), and the system cannot maintain Coherence (C). Meaning collapses. The world becomes unreadable.
This is why disorganized attachment is associated with the highest rates of psychopathology. It's not just that the person experienced trauma. It's that the trauma occurred in the context that should have been organizing—the relationship with the primary caregiver. The foundation itself is fractured.
Can Disorganized Attachment Be Repaired?
If disorganized attachment is a failure of autonomic integration—a nervous system trained in incoherence—can it be healed?
The short answer: Yes, but it's hard.
Healing disorganized attachment requires more than insight or corrective relational experience. It requires re-patterning the autonomic nervous system itself.
What Works
1. Trauma-informed therapy that targets the nervous system
Approaches like Sensorimotor Psychotherapy, Somatic Experiencing, and Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) work directly with autonomic states. The goal isn't just to process memories—it's to teach the nervous system that it can move through arousal and shutdown sequentially rather than simultaneously.
2. Polyvagal-informed interventions
Deb Dana's work on polyvagal exercises focuses on helping clients recognize their autonomic states and learn to shift between them intentionally. This involves building awareness of ventral vagal engagement (safety), recognizing sympathetic activation (mobilization), and gently working with dorsal shutdown (immobilization) without collapsing into dissociation.
3. Long-term relational repair
Disorganized attachment developed in the context of a relationship. Healing it requires a relationship that is predictable, safe, and non-threatening—something the person never had. This might be a therapist, a partner, or a close friend who can tolerate the person's dysregulation without becoming frightened or retaliating.
The key is earned security: the process by which someone with an insecure attachment history develops a secure attachment through reflection, therapy, and new relational experiences.
4. Regulation before processing
Many people with disorganized attachment histories are told to "talk about their trauma." But if the nervous system is still in simultaneous firing, talking can retraumatize. Regulation must come first. This means:
- Learning to recognize and tolerate different autonomic states - Practicing grounding and orienting to the present moment - Building a repertoire of self-soothing strategies that actually work for the person's specific nervous system - Slowly expanding the window of tolerance so that arousal or shutdown doesn't immediately trigger the other
5. EMDR and bottom-up processing
Eye Movement Desensitization and Reprocessing (EMDR) has shown efficacy for disorganized attachment because it works with the nervous system's processing mechanisms directly. By engaging bilateral stimulation while accessing traumatic material, EMDR helps the brain reprocess experiences that were stored in fragmented, incoherent ways.
What Doesn't Work
- Insight alone — Understanding your attachment style doesn't change autonomic patterns - Exposure without regulation — Pushing someone into relational closeness when their nervous system is dysregulated can reinforce the chaos - Cognitive reframing without somatic grounding — "Just change your thoughts" doesn't address the body's learned responses - Ignoring dissociation — Trying to "push through" dissociation rather than gently working with it deepens the pattern
Healing disorganized attachment is a process of re-coherencing the nervous system. It's about teaching the body that safety doesn't have to coexist with threat, that arousal can be followed by calm, that connection doesn't have to trigger shutdown.
It's possible. But it takes time, skilled guidance, and a willingness to work at the level of the nervous system—not just the mind.
The Incoherent Self
The deepest consequence of disorganized attachment is not relational chaos or emotional dysregulation, though those are real. It's the fragmentation of the self.
When the nervous system cannot form a stable attractor, identity becomes discontinuous. The person who feels safe one moment and terrified the next, who craves closeness and then flees from it, who swings between numbness and rage—this person struggles to experience themselves as a coherent whole.
This is why disorganized attachment is strongly linked to borderline personality disorder, dissociative disorders, and complex PTSD. These aren't separate conditions—they're different expressions of the same underlying incoherence. The nervous system never learned to integrate contradictory states into a stable sense of self.
But here's the paradox: the self is not an object that exists independently of the nervous system. It's an emergent property of coherent autonomic patterning. When the nervous system learns to regulate—when sympathetic arousal and dorsal shutdown stop firing simultaneously—identity begins to cohere.
This is the promise of polyvagal-informed work. It's not about fixing the self. It's about creating the conditions in which a coherent self can emerge.
Further Reading
- Main, M., & Solomon, J. (1990). "Procedures for Identifying Infants as Disorganized/Disoriented During the Ainsworth Strange Situation." Attachment in the Preschool Years. - Porges, S. W. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation. - Schore, A. N. (2003). Affect Dysregulation and Disorders of the Self. - van der Kolk, B. (2014). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. - Dana, D. (2018). The Polyvagal Theory in Therapy: Engaging the Rhythm of Regulation. - Lyons-Ruth, K., & Jacobvitz, D. (2016). "Attachment Disorganization: Genetic Factors, Parenting Contexts, and Developmental Transformation from Infancy to Adulthood." Handbook of Attachment: Theory, Research, and Clinical Applications.
This is Part 5 of the Polyvagal & Attachment series, exploring how nervous system states shape relational patterns. Next: "Secure Attachment: What Coherence Looks Like."

Comments ()