Trauma as Oscillatory Patterns
Trauma is encoded in brainstem oscillatory patterns, not cognitive content. Direct somatic interventions like breathing work and movement reshape these rhythms where insight cannot reach.
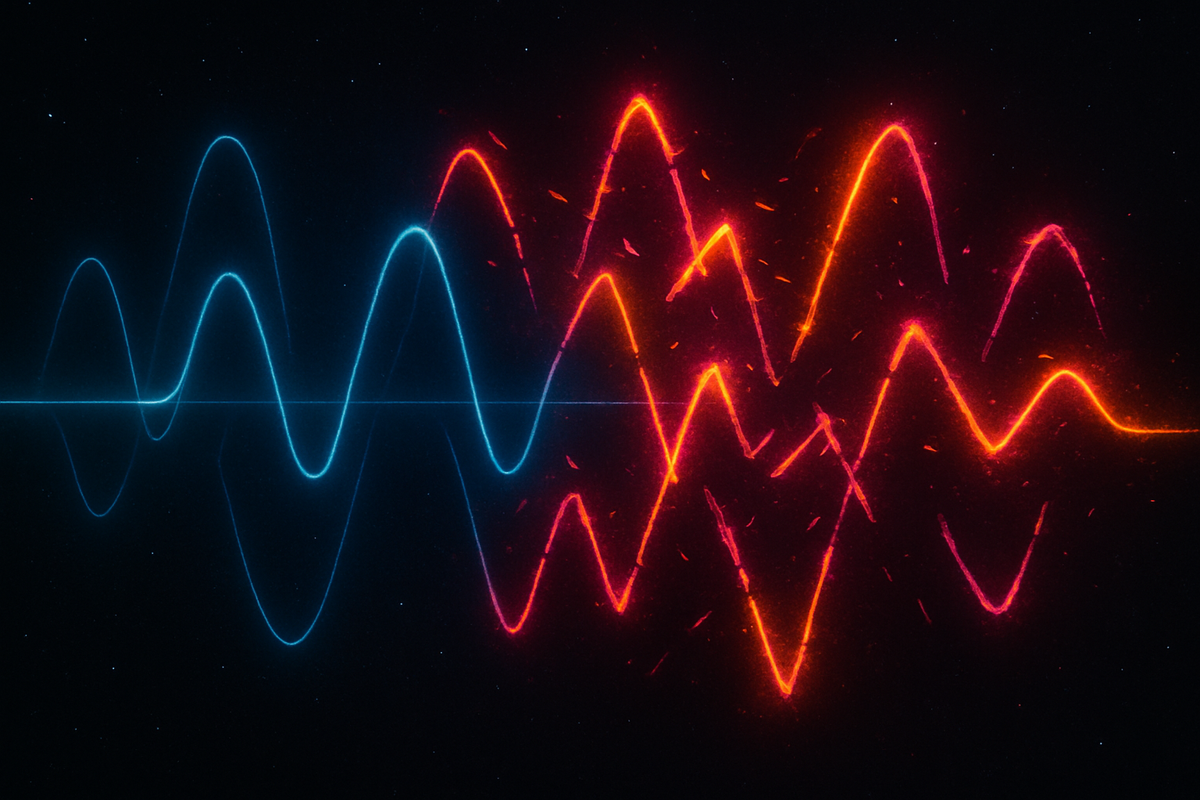
Trauma as Oscillatory Patterns
Part 9 of Polyvagal Through the Coherence LensYou cannot out-think a timing problem.This is the core insight that polyvagal theory brings to trauma. Traditional approaches often treat trauma as a content problem—wrong beliefs, disturbing memories, maladaptive thoughts. Fix the content, fix the trauma. But the nervous system doesn't store trauma as content. It stores trauma as timing.The traumatic event is over. The memory can be recalled. The danger has passed. Yet the body keeps responding as if the threat is present. Why? Because trauma lives in oscillatory patterns—in the rhythms and phase relationships that govern autonomic function. And those patterns don't update through thinking.Where Trauma LivesTrauma is not primarily stored in the hippocampus with your autobiographical memories. It's stored in:Brainstem circuits that govern autonomic response. These circuits learned, during the traumatic event, that certain cues predict danger. They continue applying that learning regardless of cortical override.Vagal tone patterns that shifted during trauma and never fully recovered. The brake that should re-engage after threat passes remains partially released.Cardiorespiratory coupling that was disrupted by overwhelming arousal and hasn't restored its coherent rhythm.Cross-frequency relationships that fragmented under extreme stress—the different timescales of the body no longer coordinating as they should.Neuroceptive thresholds that recalibrated during trauma to detect threat at lower signal levels, producing false positives in safe environments.These are timing patterns, not thoughts. They operate below the level of language. The cortex can know the threat is past. The brainstem hasn't received that memo.The Oscillatory SignatureTrauma has characteristic oscillatory signatures:Reduced HRV: The vagal brake is weakened or chronically released. Heart rate variability decreases. The flexibility that should allow rapid state transitions is compromised.Disrupted RSA: The heart-breath coupling that indicates ventral vagal function becomes attenuated or erratic. The coherent relationship between respiratory and cardiac rhythms degrades.Cross-frequency decoupling: The nested rhythms that should coordinate across timescales drift out of phase. Circadian rhythms may be disrupted. Ultradian attention cycles become erratic. The multi-scale integration breaks down.State instability: The system oscillates unpredictably between sympathetic activation and dorsal shutdown. The smooth transitions that characterize healthy autonomic function are replaced by sudden, jarring state changes.Attractor rigidity: Certain oscillatory patterns become deeply grooved—the system falls into them easily and escapes with difficulty. Hypervigilance becomes a stable attractor. Shutdown becomes a stable attractor. The healthy ventral vagal state becomes harder to access and maintain.Why Talking Doesn't Reach ItLanguage is processed cortically. Trauma lives subcortically.When you talk about trauma in traditional therapy, you're engaging prefrontal circuits—narrative construction, meaning-making, cognitive reframing. These are valuable. They can change how you think about what happened. They can update explicit beliefs. They can reduce shame and isolation.But they don't directly reach the brainstem circuits that govern autonomic response. They don't reset vagal tone. They don't restore cardiorespiratory coupling. They don't recalibrate neuroceptive thresholds.This is why someone can have complete insight into their trauma—understand it thoroughly, narrate it coherently, hold it with compassion—and still have their nervous system hijacked by a door slamming. The cortex updated. The oscillatory patterns didn't.The body doesn't speak English. It speaks rhythm.The Timing ProblemTrauma creates a timing problem in several senses:Response timing: The system responds to threat cues faster than conscious processing can intervene. By the time you think "I'm safe," the sympathetic surge has already happened. The brainstem is quicker than the cortex.Recovery timing: After activation, the system should return to baseline. In trauma, recovery is delayed or incomplete. The return to ventral vagal state takes too long or doesn't fully happen.Coupling timing: The phase relationships between oscillators are disrupted. Heart and breath don't coordinate properly. Faster and slower rhythms don't nest correctly. The timing that should integrate the system is off.Threshold timing: The system detects threat too early—responds to cues that haven't yet indicated actual danger. False positives multiply because the detection threshold has shifted.All of these are problems of when, not what. The content of the response may be appropriate—the system is doing what it's supposed to do in response to threat. But the timing is wrong. It fires too fast, recovers too slow, coordinates poorly, detects prematurely.The Coherence TranslationIn AToM terms, trauma is a deformation of the coherence manifold that persists in oscillatory structure.Curvature spikes become encoded in timing patterns. The manifold has steep regions where small cues trigger large state changes—but this steepness is maintained by the oscillatory architecture, not by conscious belief.Dimensional collapse appears as reduced oscillatory flexibility. The system can access fewer states. The range of heart rate variability narrows. The repertoire of autonomic responses shrinks.Topological fragmentation manifests as decoupling. Parts of the system that should communicate don't. Cardiac and respiratory rhythms drift apart. Different timescales stop coordinating. The integrated manifold separates into disconnected regions.Attractor capture means the system's oscillations have become trapped in particular patterns. Certain rhythms repeat because the geometry has grooved them in. Escape requires changing the groove, not just thinking differently.This is why trauma is geometric, not narrative. The shape is in the timing.What This Means for TreatmentIf trauma lives in oscillatory patterns, treatment must reach oscillatory patterns.Breathing interventions work because breath is the voluntary handle on autonomic rhythm. Structured breathing directly reshapes cardiorespiratory oscillations.Bilateral stimulation (as in EMDR) works because alternating left-right input creates a rhythmic pattern that can entrain and destabilize stuck attractors.Somatic approaches work because they engage the body's rhythms directly—pendulation, titration, discharge, and completion of defensive movements.Co-regulation works because another nervous system provides rhythmic input that can entrain a dysregulated system toward coherence.Rhythmic movement (yoga, martial arts, dance) works because it imposes external tempo that the internal oscillators can lock to.These approaches share a common feature: they address timing directly. They don't just change what you think about the trauma. They change the rhythmic patterns that constitute how trauma is held in the body.The ReframeTrauma is not a memory you can't forget. It's an oscillatory pattern you can't escape.The memory is the content. The oscillatory pattern is the structure. You can update the content—understand what happened, make meaning of it, integrate it into your narrative. But if the structure doesn't change, the body keeps responding the same way.This reframe is not pessimistic. Oscillatory patterns can change. The nervous system is plastic. Timing can be retrained. Coupling can be restored. Attractors can be reshaped.But the reframe is honest about what kind of work is required. Thinking about trauma differently is part of the process. Changing the timing patterns is another part—and it requires different interventions.You cannot out-think a timing problem. But you can out-rhythm it.Next: Three Failure Modes—distinguishing sympathetic lock, dorsal collapse, and the oscillation between them.Series: Polyvagal Through the Coherence LensArticle: 9 of 15Tags: trauma, polyvagal, oscillatory patterns, nervous system, somatic therapy
Comments ()